Sreerupa Sengupta discusses the positive and negative aspects of the risk communication strategies taken by India during COVID-19. On an international level, lessons learned from past pandemics have led to improvements in risk communication, and the Internet and social media have been used significantly to reach the public. But among other problems, use of the term “social distancing” reinforced the caste-based inequality prevalent in Indian society, Sengupta notes.
* * *
Pandemic, Risks, and Realities
History has shown that pandemics are not a novel phenomenon. Over the decades, the world has witnessed an increase in the frequency of pandemics: HIV and AIDS in 1981, SARS in 2002, swine flu in 2009, and Ebola in 2013.[1] It may sound ironic, but globalization, urbanization, environmental change, and greater mobility of people and animals have increased the potential for “global transmission of epidemics” (Hastings and Krewski 2016). While the higher frequency of pandemics has contributed to an increase in human mortality and social apprehension; pandemics have also led to transformational changes in the environment, society, and health systems research (Hall, Scott, et al. 2020). The outbreak of pandemics, such as HIV, SARS, and Ebola, has acted as a catalyst in bringing about advancements in health infrastructure, testing, screening, medical devices, medicine, and healthcare delivery. These pandemics have provided the necessary momentum and insights for reshaping risk communication during public health emergencies (WHO 2018). In short, pandemics have been our teachers. There were many lessons for the affected countries as well as for the rest of the world to leverage and strategize how to build a resilient society that can respond to public health emergencies effectively (Chatterjee, Bajwa, et al. 2020).
In March 2020, the World Health Organization (WHO) declared the outbreak of COVID-19[2] as a pandemic. The announcement of the pandemic created chaos, uncertainty, ambiguity, and anxiety across the globe. Despite experience with past pandemics and preparedness to deal with pandemics accumulated over the decades, many countries struggled to prevent and manage COVID-19 (Wang, Cleary, et al. 2020). The world was found to be in learning and reactive mode, with a greater focus on lockdown and isolation. This kind of reaction from countries was indeed surprising, especially given that it was the twenty-first century. Even risk communication during the COVID-19 pandemic created confusion and chaos in many countries.
Pandemic as Teacher: Designing Risk Communication during COVID-19
In the absence of a vaccine at the initial stage of the pandemic, countries relied heavily on nonpharmaceutical interventions (NPIs)[3] such as risk awareness to prevent and slow the transmission of the virus in the community. Risk communication emerged as one of the potent tools to make people aware of the risks, motivate them to change their behavior, and thereby control the rapid spread of the virus into the community.[4]
COVID-19 risk communication was significantly influenced by the experiences of risk communication during HIV and AIDS. HIV and COVID-19 have a few similarities. Both started with no vaccine or cure. Both pandemics created social and moral panic. Unlike COVID-19, the onslaught of HIV was slow and took nearly four decades to cause disruptions, but like COVID-19, HIV had an unprecedented impact on public health, human development, and individual lives.
HIV heralded major shifts in the discourse of health communication. HIV highlighted that individual behavior and decision-making capacity are determined by their social context and that this in turn influences their health seeking behavior (Sengupta 2013). Hence, HIV re-emphasized that the psychosocial determinants are crucial in designing realistic health messages.
Another major contribution of HIV communication was its insistence on a bottom-up approach while designing health messages to bring about social change. The significance of diverse stakeholder engagement in health communication was the point HIV drove home for policymakers, health officials, and development professionals.
Community workers, the networks of people living with HIV and AIDS activists also emphasized the necessity of risk communication to address human rights abuses that are both cause and consequence of the spread of the virus.
Taking cues from AIDS communication, the public service announcements developed by the WHO addressed the physical and emotional needs of people. The risk communication went beyond the biomedical model of health[5] and addressed an array of topics, such as empathy for people living with the virus, home care during COVID-19, stress reduction, taking care of mental health during a crisis, and provision of home care (WHO 2020). There were messages to destigmatize the disease and reduce discrimination faced by people living with the virus. The WHO also developed communication materials on how exactly to talk about the pandemic to reduce stigma and on addressing human rights as key to the response to COVID-19 (WHO 2020). The WHO acknowledged that integrating a human rights framework is “not only a moral imperative” but essential for making health communication inclusive. There were messages on the right to health of pregnant women and differently abled people and the right to life and security of healthcare workers (WHO, 2020).[6]
Social media was used extensively to send out messages on risks to a vast segment of the population. The WHO created a dedicated website on COVID-19, set up a WhatsApp group, and launched a new Information Network for Epidemics (EPI-WIN) as an immediate form of health intervention. Various countries launched national campaigns on pandemic-related issues on the government websites and social platforms to combat fake news and to encourage awareness, understanding, and compliance with government-imposed restrictions (Chatterjee, Bajwa, et al. 2020).
The risk communication developed during COVID-19 deftly incorporated the lessons learned from HIV and other health crises and brought about positive changes in the global communication on risk. The pace at which materials on risk communication developed during this pandemic in all countries and the range of topics covered is undeniably commendable.
But it should be borne in mind that while the pandemic is global, the response to it is local. As an academic and a development professional working in the domain of health communication for over a decade,[7] I became interested in exploring the changes in risk communication in India during the current public health emergency. I analyzed the risk communication materials published on social media and newspapers between March and October 2020, when cases of the novel coronavirus were sharply increasing in India.
COVID-19 Communication: Experiences from India
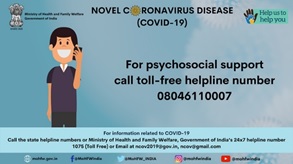
A toll-free helpline for psychosocial support.
The Ministry of Health and Family Welfare (MoHFW)[8] of India developed a plethora of information, education, and communication (IEC) materials on risk awareness related to COVID-19 and strategies to stay safe and prevent the spread of the virus. Along with print and electronic media, social media was used extensively to connect with the people; a dedicated section on COVID-19 was also developed on the website of the MoHFW. The Health Ministry networked with diverse stakeholders including departments of telecommunication, postal services, and

Educating people about rules of etiquette to follow during the pandemic.
the National Council for Science and Technology Communication to sensitize people about COVID-19. Given the paucity of time and the vast population, the government of India also joined hands with private players to reach out to remote corners of the country. For instance, the MoHFW collaborated with mobile companies to expedite the process of risk communication. Private mobile companies created ringtones to raise awareness about the virus and instructed people to report to the nearest healthcare center in case of symptoms of COVID-19. The ringtones included messages in the local languages and were aimed at debunking myths, reducing fear among the people regarding the virus, and educating them about “new normal” etiquette.
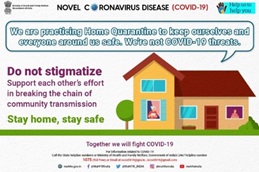
A message on home quarantine.
Given the rapid spread of the virus, multiple channels of communication, such as social and print media and mass media campaigns, were used to reach out to the people. Using multiple channels increased the chances that the intended audience will receive enough messages on risk awarene ss to absorb and act on them. It is also heartening to observe that risk awareness was not confined within the biomedical framework. Rather, the IEC materials developed by the government discussed a range of issues, such as the mental health of people living with COVID-19, empathy, home quarantine, care and support, stigma, and discrimination. The messages included, “Do not stigmatize patients and family members,” “Do not stigmatize COVID-19 survivors,” and “Standing together against COVID-19 stigma.” A psychosocial toll-free helpline and a helpline email account were created for better community engagement.
A message about destigmatizing people living with Corona.
For the first time, there was a series of communication materials that addressed the contribution of frontline workers, their need for protection, and the responsibility of society to be respectful toward them. Undoubtedly, there were major shifts in the content, channel, and strategy for risk communication during COVID-19. But notwithstanding the positive endeavor of the MoHFW, there were glaring gaps, as I outline below.
a. Uncritical acceptance of the global framework of risk communication
The MoHFW followed the diktats of the WHO in developing local risk communication materials. Hence, in most such materials developed by the national government, the term “social distancing” has been frequently used as a key risk mitigation strategy. While the WHO did initially use the term “social distancing,” it quickly switched to “physical distancing.” Unfortunately, the MoHFW upheld the globally coined language of “social distancing.” History has shown that the concept is inherently divisive. The Indian caste system thrives on the idea of social distancing. The upper caste in India maintains its purity by socially distancing themselves from the impure lower caste. Frequent usage of the concept of social distancing in risk communication reinforced and deepened the inequality prevalent in Indian society.
The concept of social distancing also assumes that people have the requisite resources and an enabling environment to adopt such preventive strategies. The critical question is: can a daily wage earner, migrant laborer, homeless person, or resident of an urban slum who lives in abject poverty realistically practice social distancing?
b. Absence of community concerns in COVID-19 communication
None of the IEC materials addressed the vulnerability of such groups as migrant laborers, homeless people, and sex workers, as if their reality does not matter. A content analysis of the posters uploaded on various social media and published in newspapers highlights the lack of representation of marginalized groups in the country. The review makes it apparent that a top-down approach had been taken in designing the risk communication materials, with little involvement of the community.
Governed by the diktats of the donors, the national government was keener to produce quantifiable results. The focus was more on measuring return on investment than on truly inducing social change. Success of risk communication was thus measured by counting the numbers of IEC materials produced, new media used, and NGOs supported in the creation of communication materials. If we observe the pattern of risk communication in India, it becomes apparent that the exercise had been an attempt to respond to the bureaucratic targets of preparing infographics, toolkits, manuals and reports rather than to uplift the lives of people and make health communication contextual, inclusive, and sustainable.
c. Failure to contextualize risk communication
HIV clearly showed that risk communication is effective only when the real concerns of the community are addressed and social norms and cultures are honored. For instance, in India, every year people suffer from measles despite vaccines. It is a common practice to quarantine the individual within the family for three weeks. Such practices neither arouse stigma nor create any panic in the community. COVID-19 communication should have made references to such health instances to allay the fear of the people, reduce their anxiety and confusion, and strike the right chord with the larger population.
Conclusion
The public health emergency in the country did usher in a number of positive changes in the landscape of risk communication. COVID-19 created the space for greater use of technology in risk communication. For a country like India, with its geographical vastness, this was indeed a boon. But the pandemic once again made it clear that to make health communication sustainable and for better risk governance, there is a need to include local words and visuals from the community in health-related materials. Health messages should use local art forms to connect with the community. Local institutions should be engaged in documenting and disseminating local and traditional practices of good health already in place, which can then be shared and practiced by diverse communities to avert pandemics. International guidelines provide a direction to risk communication, but risk communication should essentially be context specific and people centered. Unless that happens, risk communication will remain a tool for public health management and not an initiative for the people to claim their right to health.
Adapted by the author from an article originally posted on changeframing.space: https://www.changeframing.space/answering-the-burning-questions/confusion-angst-and-deceptive-communication.
[1] The world witnessed the outbreak of HIV and AIDS in 1981 in the United States. Over the decades, HIV spread to several countries. Severe Acute Respiratory Syndrome (SARS, 2002–2003) originated in China and spread to nearly 29 countries, swine flu (2009–2010) appeared in Mexico and spread to at least 30 countries, and Ebola (2013–2014) appeared in Africa and spread to at least 10 countries. It was the geographical spread of these viruses that earned them the title of pandemic. The number of people affected by the latter three viruses did not reach the proportion of either HIV or the current COVID-19. See https://www.changeframing.space/answering-the-burning-questions/confusion-angst-and-deceptive-communication.
[2] COVID-19 is the infectious disease caused by the most recently discovered coronavirus. This new virus and disease were unknown before the outbreak began in Wuhan, China, in December 2019. COVID-19 is now a pandemic affecting many countries globally. See https://www.who.int/emergencies/diseases/novel-coronavirus-2019.
[3] According to the US Centers for Disease Control and Prevention (CDC), nonpharmaceutical interventions are actions that people and communities can take to help slow the spread of illnesses like pandemic influenza in the absence of a vaccine or medicine. NPIs are also known as community mitigation strategies. See https://www.cdc.gov/nonpharmaceutical-interventions/index.html.
[4] Risk communication forms an essential component in the package of effective pandemic response. In 2005, the International Health Regulations underscored its importance as a health intervention. Since then, risk communication has become central to the WHO’s Pandemic Influenza Preparedness Framework (WHO 2018).
[5] The biomedical approach focuses on disease transmission and prevention from a clinical perspective. Risk communication following a biomedical model of health will discuss only transmission of the virus and methods of prevention; the focus is only on biological factors. Other factors, such as psychological, environmental, and social, are not taken into consideration.
[6] See https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public.
[7] My affair with health communication happened in 2006 through a project on HIV and violence against women (VAW). Thereafter, the Sasakawa Young Leaders Fellowship Fund (Sylff) fellowship in 2008 gave me an opportunity to delve into the politics and ideology that influence health messages and engage with the community to make health communication more inclusive. My doctoral dissertation adopted a gender- and rights-based approach to analyze representation of gender inequality, HIV, and human rights and the intersections between them in HIV-related communication in India.
[8] The Ministry of Health and Family Welfare (https://main.mohfw.gov.in/about-us/about-the-ministry) is responsible for health policy and the planning and implementation of health-related programs in India. The ministry also looks into matters pertaining to family planning in India.
References
Chatterjee, R, S. Bajwa, D. Dwivedi, et al. 2020. “COVID-19 Risk Assessment Tool: Dual Application of Risk Communication and Risk Governance.” Progress in Disaster Science 7 (October 2020), 1–11. https://doi.org/10.1016/j.pdisas.2020.100109.
Hall, C., D. Scott, and S. Gössling. 2020. “Pandemics, Transformations and Tourism: Be Careful What You Wish For.” Tourism Geographies 22, no. 3 (2020),577-598 https://doi.org/10.1080/14616688.2020.1759131.
International Labour Organization. 2020. An Employer’s Guide on Working from Home in Response to the Outbreak of COVID-19. https://www.ilo.org/wcmsp5/groups/public/---ed_dialogue/---act_emp/documents/publication/wcms_745024.pdf.
Saunders-Hastings, Patrick R., and Daniel Krewski. 2016. “Reviewing the History of Pandemic Influenza: Understanding Patterns of Emergence and Transmission.” Pathogens 5, no. 4 (2016), 66 https://doi.org/10.3390/pathogens5040066
Sengupta, S. 2013. HIV and AIDS Media Campaigns in India: Exploring Issues of Gender and Rights, Doctoral Dissertation, Jadavpur University, 2013. http://hdl.handle.net/10603/133048
Wang, H., P. Cleary, J. Little, et al. 2020. “Communicating in a Public Health Crisis”. The Lancet Digital Health 2, no. 10 (2020): e503. https://doi.org/10.1016/S2589-7500(20)30197-7.
World Health Organization (WHO). 2020. Gender and COVID-19: Advocacy Brief. https://apps.who.int/iris/bitstream/handle/10665/332080/WHO-2019-nCoV-Advocacy_brief-Gender-2020.1-eng.pdf?sequence=1&isAllowed=y.
WHO. 2020. Addressing Human Rights as Key to the COVID-19 Response. https://www.who.int/publications/i/item/addressing-human-rights-as-key-to-the-covid-19-response.
WHO. 2018. Communicating Risk in Public Health Emergencies: A WHO Guideline for Emergency Risk Communication (ERC) Policy and Practice. https://apps.who.int/iris/bitstream/handle/10665/259807/9789241550208-eng.pdf?sequence=2.
WHO. Coronavirus Disease (COVID-19) Advice for the Public. Last updated April 9, 2021. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public.




